Diabetes 1, also known as juvenile diabetes or insulin-dependent diabetes, is a chronic autoimmune disease that affects the pancreas. In diabetes 1, the pancreas produces little or no insulin, a hormone that helps glucose, or sugar, get from the blood into the cells of the body for energy. Without insulin, blood sugar levels can get too high, leading to a number of health problems.
Treatment for diabetes 1 typically involves taking insulin, either through injections or an insulin pump. Insulin helps to lower blood sugar levels and keep them in a healthy range. Other treatments for diabetes 1 may include diet and exercise, as well as monitoring blood sugar levels regularly.
Diabetes 1 is a serious disease, but it can be managed with proper treatment. People with diabetes 1 can live long, healthy lives by following their treatment plan and making healthy lifestyle choices.
Diabetes 1 Treatment
Diabetes 1 treatment is essential for managing blood sugar levels and preventing serious health complications. There are several key aspects to diabetes 1 treatment, including:
- Insulin therapy: Insulin is a hormone that helps glucose get from the blood into the cells of the body for energy. People with diabetes 1 need to take insulin to lower their blood sugar levels.
- Blood sugar monitoring: People with diabetes 1 need to monitor their blood sugar levels regularly to make sure they are in a healthy range.
- Diet: Eating a healthy diet can help people with diabetes 1 manage their blood sugar levels.
- Exercise: Exercise can help people with diabetes 1 lower their blood sugar levels and improve their overall health.
- Medications: In addition to insulin, people with diabetes 1 may also need to take other medications to manage their blood sugar levels.
- Education: Learning about diabetes 1 and its treatment is essential for people with diabetes 1 to manage their condition.
- Support: People with diabetes 1 can benefit from support from family, friends, and healthcare providers.
- Technology: There are a number of technologies available to help people with diabetes 1 manage their condition, such as insulin pumps and continuous glucose monitors.
These are just some of the key aspects of diabetes 1 treatment. By following their treatment plan and making healthy lifestyle choices, people with diabetes 1 can live long, healthy lives.
Insulin therapy
Insulin therapy is a cornerstone of diabetes 1 treatment. Without insulin, people with diabetes 1 cannot survive. Insulin therapy helps to lower blood sugar levels and keep them in a healthy range.
- Types of insulin therapy: There are several different types of insulin therapy, including injections, insulin pumps, and inhaled insulin. The type of insulin therapy that is best for a person with diabetes 1 will depend on their individual needs and preferences.
- Dosing insulin: The dose of insulin that a person with diabetes 1 needs will vary depending on their blood sugar levels, diet, and activity level. It is important to work with a healthcare provider to determine the correct dose of insulin.
- Monitoring blood sugar levels: People with diabetes 1 need to monitor their blood sugar levels regularly to make sure they are in a healthy range. This can be done using a blood glucose meter.
- Complications of insulin therapy: Insulin therapy can sometimes cause side effects, such as hypoglycemia (low blood sugar) and weight gain. It is important to be aware of these side effects and to work with a healthcare provider to manage them.
Insulin therapy is an essential part of diabetes 1 treatment. By following their insulin therapy plan, people with diabetes 1 can live long, healthy lives.
Blood sugar monitoring
Blood sugar monitoring is an essential part of diabetes 1 treatment. By monitoring their blood sugar levels, people with diabetes 1 can make sure that their blood sugar levels are in a healthy range and take steps to correct them if they are not.
There are two main types of blood sugar monitoring: self-monitoring of blood glucose (SMBG) and continuous glucose monitoring (CGM). SMBG involves using a blood glucose meter to measure blood sugar levels at specific times throughout the day. CGM involves wearing a small sensor that measures blood sugar levels continuously and transmits the data to a receiver or mobile device.
Both SMBG and CGM can be used to effectively manage blood sugar levels. However, CGM may be more convenient and accurate for some people with diabetes 1. CGM can also help to prevent hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar) by providing real-time data on blood sugar levels.
Blood sugar monitoring is an essential part of diabetes 1 treatment. By monitoring their blood sugar levels, people with diabetes 1 can make sure that their blood sugar levels are in a healthy range and take steps to correct them if they are not.
Diet
Diet is an essential part of diabetes 1 treatment. Eating a healthy diet can help people with diabetes 1 manage their blood sugar levels and reduce their risk of developing complications.
There are a few key things to keep in mind when creating a healthy diet for diabetes 1. First, it is important to eat regular meals and snacks throughout the day. This will help to keep blood sugar levels stable. Second, it is important to choose foods that are low in carbohydrates. Carbohydrates are broken down into glucose in the body, which can raise blood sugar levels. Third, it is important to choose foods that are high in fiber. Fiber helps to slow down the absorption of glucose into the bloodstream, which can also help to keep blood sugar levels stable.
Some good examples of foods that are good for people with diabetes 1 include:
- Fruits and vegetables
- Whole grains
- Lean protein
- Low-fat dairy
It is also important to avoid foods that are high in sugar, saturated fat, and trans fat. These foods can raise blood sugar levels and increase the risk of developing complications.
Following a healthy diet is an essential part of diabetes 1 treatment. By eating a healthy diet, people with diabetes 1 can manage their blood sugar levels and reduce their risk of developing complications.
Exercise
Exercise is an important part of diabetes 1 treatment. Exercise can help to lower blood sugar levels, improve insulin sensitivity, and reduce the risk of developing complications. Regular exercise can also help to improve overall health and well-being.
When people with diabetes 1 exercise, their muscles use glucose for energy. This can help to lower blood sugar levels. Exercise also helps to improve insulin sensitivity, which means that the body’s cells are better able to use insulin to take glucose from the blood. This can also help to lower blood sugar levels.
In addition to lowering blood sugar levels, exercise can also help to improve overall health and well-being. Exercise can help to strengthen the heart and lungs, improve circulation, and reduce stress. Exercise can also help to improve sleep quality and mood.There are many different types of exercise that people with diabetes 1 can enjoy. Some good choices include walking, swimming, biking, and strength training. It is important to start slowly and gradually increase the intensity and duration of exercise over time. People with diabetes 1 should always talk to their doctor before starting an exercise program.Exercise is an important part of diabetes 1 treatment. By exercising regularly, people with diabetes 1 can lower their blood sugar levels, improve their overall health, and reduce their risk of developing complications.
Medications
Medications play a crucial role in diabetes 1 treatment, alongside insulin therapy. These medications work in various ways to regulate blood sugar levels, addressing specific aspects of diabetes management.
-
Blood Glucose-Lowering Medications:
These medications, such as metformin and sulfonylureas, stimulate the pancreas to produce more insulin or increase the body’s sensitivity to insulin. They help lower blood sugar levels, particularly after meals.
-
Amylin Analogs:
Pramlintide is an injectable medication that mimics the hormone amylin, which helps slow down stomach emptying and reduce post-meal blood sugar spikes.
-
Sodium-Glucose Cotransporter 2 (SGLT2) Inhibitors:
Medications like empagliflozin and canagliflozin block SGLT2 in the kidneys, leading to increased glucose excretion in the urine, resulting in lower blood sugar levels.
-
Glucagon-Like Peptide-1 (GLP-1) Receptor Agonists:
These injectable medications, such as exenatide and liraglutide, stimulate GLP-1 receptors, promoting insulin secretion, slowing stomach emptying, and suppressing appetite.
The choice of medications depends on individual patient needs, blood sugar control, and other factors. Medications can be used in combination with insulin to achieve optimal glycemic control and reduce the risk of complications associated with diabetes 1.
Education
Education is a cornerstone of successful diabetes 1 treatment. It empowers individuals with the knowledge and skills necessary to manage their condition effectively, leading to improved health outcomes and a better quality of life.
- Understanding Diabetes 1: Education begins with a thorough understanding of diabetes 1, its causes, symptoms, and potential complications. This knowledge helps individuals recognize the warning signs of high or low blood sugar levels and take appropriate action.
- Insulin Management: People with diabetes 1 rely on insulin therapy to manage their blood sugar levels. Education covers the proper techniques for insulin injection, storage, and dosage adjustment based on blood sugar monitoring and lifestyle factors.
- Blood Sugar Monitoring: Regular blood sugar monitoring is crucial for effective diabetes 1 management. Education emphasizes the use of blood glucose meters, interpretation of results, and the importance of keeping a log to track patterns and adjust treatment accordingly.
- Dietary Management: Nutrition plays a vital role in diabetes 1 management. Education focuses on healthy eating habits, including meal planning, carbohydrate counting, and understanding the impact of food choices on blood sugar levels.
Education empowers people with diabetes 1 to become active participants in their own care. It fosters self-management skills, promotes healthy behaviors, and ultimately leads to improved blood sugar control, reduced risk of complications, and enhanced quality of life.
Support
Support from family, friends, and healthcare providers is a crucial component of effective diabetes 1 treatment. It provides emotional, practical, and informational resources that empower individuals to manage their condition and improve their well-being.
Emotional Support: Diabetes 1 can be a challenging and isolating condition. Support from loved ones can provide a sense of understanding, empathy, and encouragement. Family and friends can offer companionship, listen to concerns, and help individuals cope with the emotional burden of living with a chronic illness.
Practical Assistance: Support systems can provide practical assistance with tasks related to diabetes management, such as meal preparation, medication administration, and blood sugar monitoring. This assistance can help individuals maintain a healthy lifestyle and adhere to their treatment plan, ultimately improving their health outcomes.
Healthcare Collaboration: Healthcare providers play a vital role in providing medical care, education, and support to individuals with diabetes 1. They work in collaboration with support systems to ensure a comprehensive and coordinated approach to treatment. Regular appointments, open communication, and access to healthcare professionals empower individuals to make informed decisions and effectively manage their condition.
The connection between support and diabetes 1 treatment is evident in its positive impact on various aspects of disease management. Support systems can improve adherence to treatment plans, reduce the risk of complications, and enhance overall quality of life for individuals with diabetes 1.
Technology
The advancement of technology has revolutionized diabetes 1 treatment, providing individuals with innovative tools to effectively manage their condition. Insulin pumps and continuous glucose monitors (CGMs) are prime examples of these technologies, offering significant benefits in blood sugar regulation and overall well-being.
Insulin pumps deliver insulin continuously or at programmed intervals, mimicking the body’s natural insulin production. This method provides more precise insulin delivery compared to multiple daily injections, resulting in better blood sugar control and reduced risk of hypoglycemia (low blood sugar). Insulin pumps also offer flexibility and convenience, allowing individuals to adjust insulin doses based on their activities, meals, and blood sugar levels.
CGMs monitor glucose levels continuously, providing real-time data and alerts. This information empowers individuals to make informed decisions about insulin dosing, diet, and exercise, enabling proactive management of blood sugar levels. CGMs have been shown to improve glycemic control, reduce hypoglycemia risk, and enhance overall quality of life.
The integration of technology into diabetes 1 treatment has significantly improved disease management. Insulin pumps and CGMs provide greater precision, flexibility, and real-time monitoring, empowering individuals to achieve optimal blood sugar control and minimize complications associated with diabetes 1.
FAQs on Diabetes 1 Treatment
Diabetes 1 treatment involves managing blood sugar levels through insulin therapy, diet, exercise, medication, and support systems. Here are answers to some frequently asked questions about diabetes 1 treatment:
Question 1: What is the main goal of diabetes 1 treatment?
The primary goal of diabetes 1 treatment is to maintain healthy blood sugar levels within a target range. This helps prevent both immediate symptoms and long-term complications associated with diabetes.
Question 2: How is insulin used in diabetes 1 treatment?
Insulin is a hormone that helps glucose enter cells for energy. In diabetes 1, the body does not produce insulin, so insulin therapy is essential to regulate blood sugar levels. Insulin can be administered through injections, an insulin pump, or an inhaled form.
Question 3: What dietary changes are recommended for people with diabetes 1?
A healthy diet for diabetes 1 involves regular meals and snacks, focusing on nutrient-rich foods such as fruits, vegetables, whole grains, and lean protein. Limiting processed foods, sugary drinks, and saturated fats is also important.
Question 4: How does exercise impact diabetes 1 treatment?
Regular exercise helps improve insulin sensitivity and blood sugar control in people with diabetes 1. It is recommended to engage in moderate-intensity exercise for at least 150 minutes per week.
Question 5: What are the different types of medications used in diabetes 1 treatment?
In addition to insulin, other medications may be prescribed to manage blood sugar levels, such as metformin, sulfonylureas, and GLP-1 receptor agonists. These medications work by increasing insulin production, enhancing insulin sensitivity, or slowing down the absorption of glucose.
Question 6: How often should blood sugar levels be monitored in diabetes 1?
Blood sugar monitoring is crucial for effective diabetes 1 management. The frequency of monitoring may vary depending on individual needs and treatment plan, but regular checks throughout the day, including before and after meals, are generally recommended.
These FAQs provide a general overview of diabetes 1 treatment. It is essential to consult with a healthcare professional for personalized guidance and a comprehensive treatment plan.
Transition to the next article section:
Tips for Managing Diabetes 1 Effectively
Living with diabetes 1 requires ongoing management to maintain blood sugar levels within a healthy range. Here are several tips to assist individuals in effectively managing their condition:
Tip 1: Monitor Blood Sugar RegularlyRegular blood sugar monitoring is essential for understanding blood sugar patterns and making necessary adjustments to insulin doses and lifestyle. It helps prevent both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar).Tip 2: Follow a Healthy DietMaintaining a balanced diet is crucial for diabetes 1 management. Focus on nutrient-rich foods such as fruits, vegetables, whole grains, and lean protein. Limit processed foods, sugary drinks, and unhealthy fats to maintain stable blood sugar levels.Tip 3: Engage in Regular ExerciseExercise improves insulin sensitivity and blood sugar control. Aim for at least 150 minutes of moderate-intensity exercise per week. Physical activity helps utilize glucose for energy, reducing blood sugar levels.Tip 4: Take Medications as PrescribedIn addition to insulin, other medications may be prescribed to manage blood sugar levels. Take medications exactly as directed, even if feeling well, to maintain optimal blood sugar control and prevent complications.Tip 5: Prioritize SleepAdequate sleep is essential for overall health, including diabetes management. Aim for 7-9 hours of quality sleep each night. Sleep deprivation can affect insulin sensitivity, making blood sugar control more challenging.Tip 6: Manage StressStress can trigger hormone responses that elevate blood sugar levels. Find healthy ways to manage stress, such as exercise, yoga, or meditation. Stress management techniques can improve blood sugar control and overall well-being.Tip 7: Quit SmokingSmoking negatively impacts blood sugar control and increases the risk of diabetes complications. Quitting smoking is crucial for improving overall health and diabetes management.Tip 8: Get Regular Check-upsRegular check-ups with a healthcare professional are essential for monitoring diabetes management, adjusting treatment plans, and preventing complications. Open communication and collaboration with healthcare providers optimize outcomes.
Diabetes 1 Treatment
Diabetes 1 treatment encompasses a multifaceted approach to regulating blood sugar levels and preventing complications. Insulin therapy remains the cornerstone of treatment, complemented by dietary modifications, regular exercise, and medications as needed. Effective management requires a comprehensive understanding of the condition, proper monitoring, and adherence to treatment plans.
Empowering individuals with knowledge, support systems, and advanced technologies optimizes diabetes 1 management. Continuous glucose monitors and insulin pumps provide real-time data and precise insulin delivery, enhancing blood sugar control and reducing the risk of complications. Support from family, friends, and healthcare professionals fosters emotional well-being, practical assistance, and collaborative decision-making.
Diabetes 1 treatment is an ongoing journey, requiring commitment, resilience, and a collaborative effort between individuals and healthcare providers. By embracing a proactive approach, adopting healthy lifestyle choices, and utilizing available resources, people with diabetes 1 can lead fulfilling and active lives.
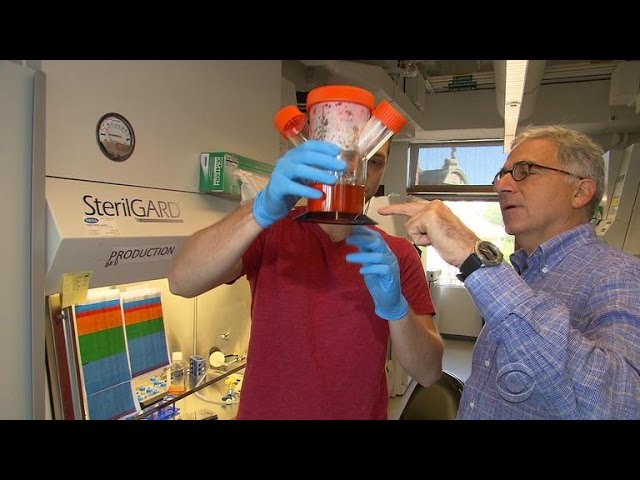
Youtube Video: