Diabetic mastopathy refers to breast tissue changes linked to diabetes. It typically occurs in women with long-standing, poorly controlled diabetes and is characterized by the presence of dense, fibrous tissue within the breasts.
The exact cause of diabetic mastopathy is not fully understood, but it is believed to be related to the effects of high blood sugar levels on the breast tissue. Over time, elevated blood sugar can damage the delicate blood vessels in the breasts, leading to the development of fibrous tissue and the formation of breast lumps.
Diabetic mastopathy is generally not a cause for concern and does not increase the risk of breast cancer. However, it can make it more difficult to detect breast cancer through mammograms, as the dense breast tissue can obscure the presence of tumors. Therefore, women with diabetic mastopathy may need to undergo more frequent mammograms or consider alternative breast imaging techniques, such as breast MRI or ultrasound.
diabetic mastopathy
Diabetic mastopathy involves breast tissue changes associated with diabetes, presenting as dense, fibrous breast tissue. Understanding its various dimensions is crucial for proper diagnosis and management. Key aspects to consider include:
- Pathophysiology: High blood sugar damages breast blood vessels, leading to fibrosis.
- Clinical presentation: Dense breasts, palpable lumps, and mammographic abnormalities.
- Differential diagnosis: Distinguishing from other breast conditions, including cancer.
- Management: Regular breast exams, mammograms, and potential MRI or ultrasound.
- Monitoring: Tracking breast changes and response to treatment.
- Patient education: Informing patients about the condition and its implications.
- Research: Ongoing studies to better understand causes and improve diagnosis.
- Awareness: Raising awareness among healthcare professionals and the public.
These aspects highlight the importance of recognizing diabetic mastopathy, its clinical presentation, and the need for appropriate management and monitoring. By understanding these dimensions, healthcare providers can better assist patients with diabetes in maintaining breast health and addressing any related concerns.
Pathophysiology
Diabetic mastopathy is a condition that affects the breast tissue of women with diabetes. It is characterized by the presence of dense, fibrous tissue in the breasts. This fibrosis is caused by high blood sugar levels, which damage the blood vessels in the breasts. The damaged blood vessels lead to the accumulation of fluid and the formation of fibrous tissue.
The pathophysiology of diabetic mastopathy is important to understand because it helps to explain the symptoms and the potential complications of the condition. The fibrosis can make the breasts feel lumpy and tender, and it can also make it more difficult to detect breast cancer on mammograms. In some cases, diabetic mastopathy can also lead to breast pain and nipple discharge.
There is no cure for diabetic mastopathy, but the condition can be managed with lifestyle changes and medication. Lifestyle changes that can help to improve diabetic mastopathy include controlling blood sugar levels, eating a healthy diet, and exercising regularly. Medications that can help to reduce the fibrosis include tamoxifen and raloxifene.
Clinical presentation
The clinical presentation of diabetic mastopathy includes dense breasts, palpable lumps, and mammographic abnormalities. Dense breasts are a common finding in women with diabetes, and they can make it more difficult to detect breast cancer on mammograms. Palpable lumps are another common finding in women with diabetic mastopathy, and they can be a sign of breast cancer or other breast conditions. Mammographic abnormalities are also common in women with diabetic mastopathy, and they can include changes in the breast tissue, such as calcifications or masses.
The clinical presentation of diabetic mastopathy is important to understand because it can help to diagnose and manage the condition. Dense breasts, palpable lumps, and mammographic abnormalities can all be signs of breast cancer, so it is important to have these symptoms evaluated by a doctor. In addition, the clinical presentation of diabetic mastopathy can help to guide treatment decisions. For example, women with dense breasts may need to have more frequent mammograms or consider alternative breast imaging techniques, such as breast MRI or ultrasound.
The clinical presentation of diabetic mastopathy is a complex and challenging issue. However, by understanding the connection between the clinical presentation and the underlying pathophysiology, healthcare providers can better diagnose and manage the condition.
Differential diagnosis
Diabetic mastopathy can sometimes mimic other breast conditions, including cancer, making accurate diagnosis crucial. Differential diagnosis involves distinguishing diabetic mastopathy from these other conditions to ensure appropriate management. Key considerations include:
- Clinical presentation: While diabetic mastopathy typically presents with dense breasts and palpable lumps, other conditions may have distinct clinical features, such as skin changes, nipple discharge, or axillary lymphadenopathy.
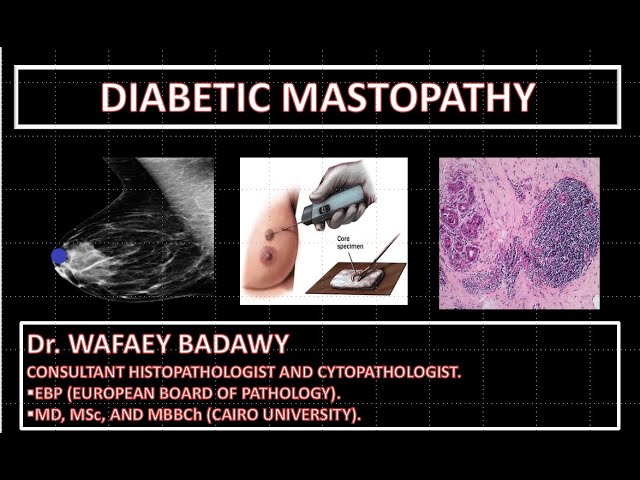
- Imaging findings: Mammograms and other imaging modalities can help differentiate diabetic mastopathy from other breast lesions. For instance, cancer may present with specific mammographic characteristics like spiculated margins or microcalcifications.
- Histopathology: In some cases, a biopsy may be necessary to definitively distinguish diabetic mastopathy from cancer or other breast conditions. Microscopic examination of breast tissue can provide a definitive diagnosis.
- Patient history: A thorough medical and family history can provide valuable clues. A history of diabetes, duration, and control can support the diagnosis of diabetic mastopathy, while a personal or family history of breast cancer may warrant further investigation.
Accurate differential diagnosis is essential to avoid unnecessary procedures, provide appropriate treatment, and ensure optimal patient outcomes. By carefully considering the clinical presentation, imaging findings, histopathology, and patient history, healthcare providers can effectively distinguish diabetic mastopathy from other breast conditions, including cancer.
Management
Management of diabetic mastopathy involves regular breast exams, mammograms, and potential MRI or ultrasound examinations. These measures are crucial for monitoring breast health, detecting abnormalities, and ensuring timely intervention.
- Regular breast exams: Self-breast exams and clinical breast exams by a healthcare professional allow for the detection of lumps or other changes in breast tissue. This practice promotes early detection of any abnormalities that may require further evaluation.
- Mammograms: Mammograms use low-dose X-rays to create images of the breast tissue, aiding in the identification of masses or calcifications that may indicate underlying breast conditions, including cancer.
- MRI or ultrasound: In certain cases, MRI (magnetic resonance imaging) or ultrasound may be recommended as complementary imaging techniques. MRI provides detailed cross-sectional images of the breast, while ultrasound uses sound waves to create real-time images, both of which can enhance the detection and characterization of breast lesions.
Regular monitoring and appropriate imaging are essential for managing diabetic mastopathy. By adhering to these recommendations, women with diabetes can proactively care for their breast health, promptly address any concerns, and minimize the risk of complications.
Monitoring
Monitoring breast changes and response to treatment is a crucial component of managing diabetic mastopathy. Regular monitoring allows healthcare providers to assess the effectiveness of treatment, detect any, and make necessary adjustments to the treatment plan.
There are several methods used to monitor breast changes in women with diabetic mastopathy. These include:
- Clinical breast exams: Regular clinical breast exams by a healthcare professional can help detect lumps or other changes in breast tissue. This is an important screening method for detecting breast cancer and other breast conditions.
- Mammograms: Mammograms use low-dose X-rays to create images of the breast tissue, aiding in the identification of masses or calcifications that may indicate underlying breast conditions, including cancer.
- MRI or ultrasound: In certain cases, MRI (magnetic resonance imaging) or ultrasound may be recommended as complementary imaging techniques. MRI provides detailed cross-sectional images of the breast, while ultrasound uses sound waves to create real-time images, both of which can enhance the detection and characterization of breast lesions.
- Patient self-exams: Women with diabetic mastopathy are encouraged to perform regular breast self-exams to monitor for any changes in their breasts. This practice can help detect abnormalities early on, allowing for prompt medical evaluation.
By carefully monitoring breast changes and response to treatment, healthcare providers can ensure that women with diabetic mastopathy receive the most appropriate care. Regular monitoring can help to prevent complications, detect breast cancer early, and improve overall breast health outcomes.
Patient education
Patient education is a crucial aspect of managing diabetic mastopathy. It involves providing patients with comprehensive information about the condition, its implications, and the available treatment options. Effective patient education empowers individuals to make informed decisions regarding their health and actively participate in their care.
- Understanding the condition: Patients should be educated about the nature of diabetic mastopathy, its causes, and its potential impact on breast health. This includes explaining the link between diabetes and breast tissue changes, the development of dense breast tissue, and the increased risk of breast cancer.
- Symptoms and monitoring: Patients should be informed about the common symptoms of diabetic mastopathy, such as breast lumps, thickening, and tenderness. They should also be instructed on the importance of regular breast self-exams and clinical breast exams to monitor for any changes in breast tissue.
- Treatment options: Patients should be made aware of the available treatment options for diabetic mastopathy, including lifestyle modifications, medications, and surgical interventions. The benefits and risks of each treatment option should be thoroughly discussed to help patients make informed choices.
- Lifestyle modifications: Patients should be counseled on the importance of lifestyle modifications to manage diabetic mastopathy. This includes controlling blood sugar levels, maintaining a healthy weight, and engaging in regular exercise. These measures can help reduce the risk of breast cancer and improve overall health outcomes.
Effective patient education is essential for empowering patients with diabetic mastopathy to take an active role in their care. By providing comprehensive information and support, healthcare providers can enable patients to make informed decisions, adhere to treatment plans, and improve their overall breast health outcomes.
Research
Research into diabetic mastopathy is ongoing, with studies aiming to better understand the causes of the condition and improve its diagnosis. This research is important because it can lead to the development of new treatments and preventive measures for diabetic mastopathy, which can ultimately improve the health outcomes of women with diabetes.
- Identifying risk factors: Researchers are working to identify the risk factors for diabetic mastopathy, such as the duration of diabetes, blood sugar control, and genetic factors. This information can help to identify women who are at high risk for developing the condition and who may need more frequent screening.
- Developing new imaging techniques: Researchers are also developing new imaging techniques to improve the diagnosis of diabetic mastopathy. These techniques may be able to detect the condition earlier and more accurately, which can lead to earlier treatment and better outcomes.
- Studying the role of lifestyle factors: Researchers are also studying the role of lifestyle factors in diabetic mastopathy. This research is looking at how diet, exercise, and other lifestyle factors may affect the development and progression of the condition.
- Developing new treatments: Researchers are also developing new treatments for diabetic mastopathy. These treatments may include medications, surgery, or lifestyle changes. The goal of these treatments is to reduce the symptoms of diabetic mastopathy and prevent the development of breast cancer.
The research on diabetic mastopathy is ongoing, and new findings are emerging all the time. This research is important for improving the health outcomes of women with diabetes and for preventing the development of breast cancer.
Awareness
Raising awareness about diabetic mastopathy among healthcare professionals and the public is crucial for improving the diagnosis and management of this condition. Increased awareness can lead to earlier detection, appropriate treatment, and better outcomes for women with diabetes.
- Educating healthcare professionals: Many healthcare professionals may not be familiar with diabetic mastopathy, which can lead to misdiagnosis or delayed diagnosis. Raising awareness among healthcare professionals can help ensure that they are knowledgeable about the condition and can provide appropriate care to their patients.
- Empowering women with diabetes: Women with diabetes need to be aware of the potential risk of diabetic mastopathy and the importance of regular breast exams and mammograms. Raising awareness can help women to be proactive about their breast health and to seek medical attention if they notice any changes in their breasts.
- Reducing stigma: Diabetic mastopathy can sometimes be associated with shame or embarrassment. Raising awareness can help to reduce the stigma surrounding the condition and encourage women to seek help if they are experiencing symptoms.
- Promoting research: Increased awareness can lead to more funding for research into diabetic mastopathy. This research can help to improve our understanding of the condition and to develop new treatments.
Raising awareness about diabetic mastopathy is a critical step towards improving the health of women with diabetes. By educating healthcare professionals, empowering women, reducing stigma, and promoting research, we can work together to ensure that women with diabetic mastopathy receive the care they need.
Frequently Asked Questions about Diabetic Mastopathy
This section addresses frequently asked questions (FAQs) about diabetic mastopathy, providing concise and informative answers to common concerns and misconceptions.
Question 1: What is diabetic mastopathy?
Answer: Diabetic mastopathy is a condition that affects the breast tissue of women with diabetes. It is characterized by the presence of dense, fibrous tissue in the breasts, which can make it more difficult to detect breast cancer on mammograms.
Question 2: What causes diabetic mastopathy?
Answer: Diabetic mastopathy is caused by high blood sugar levels, which damage the blood vessels in the breasts. The damaged blood vessels lead to the accumulation of fluid and the formation of fibrous tissue.
Question 3: What are the symptoms of diabetic mastopathy?
Answer: The most common symptom of diabetic mastopathy is dense breasts. Other symptoms may include palpable lumps, breast pain, and nipple discharge.
Question 4: How is diabetic mastopathy diagnosed?
Answer: Diabetic mastopathy is diagnosed based on a physical examination of the breasts and a mammogram. In some cases, a biopsy may be necessary to confirm the diagnosis.
Question 5: How is diabetic mastopathy treated?
Answer: There is no cure for diabetic mastopathy, but the condition can be managed with lifestyle changes and medication. Lifestyle changes that can help to improve diabetic mastopathy include controlling blood sugar levels, eating a healthy diet, and exercising regularly.
Question 6: What is the prognosis for diabetic mastopathy?
Answer: The prognosis for diabetic mastopathy is generally good. However, women with diabetic mastopathy have an increased risk of developing breast cancer. Therefore, it is important for women with diabetic mastopathy to have regular breast exams and mammograms.
Summary: Diabetic mastopathy is a common condition that affects women with diabetes. It is important to be aware of the symptoms of diabetic mastopathy and to have regular breast exams and mammograms to ensure early detection and treatment.
Transition to the next article section: For more information on diabetic mastopathy, please consult with your healthcare provider or visit a reputable medical website.
Tips for Managing Diabetic Mastopathy
Diabetic mastopathy is a condition that can affect women with diabetes. It is characterized by the presence of dense, fibrous tissue in the breasts, which can make it more difficult to detect breast cancer on mammograms. While there is no cure for diabetic mastopathy, there are a number of things that women can do to manage the condition and reduce their risk of breast cancer.
Tip 1: Control blood sugar levels. High blood sugar levels can damage the blood vessels in the breasts, leading to the development of diabetic mastopathy. Controlling blood sugar levels can help to prevent or slow the progression of the condition.
Tip 2: Eat a healthy diet. Eating a healthy diet can help to maintain a healthy weight and reduce the risk of developing diabetes and other chronic diseases. A healthy diet includes plenty of fruits, vegetables, and whole grains.
Tip 3: Exercise regularly. Exercise can help to improve blood sugar control and reduce the risk of developing diabetes and other chronic diseases. Exercise also helps to maintain a healthy weight.
Tip 4: Get regular breast exams and mammograms. Women with diabetic mastopathy should have regular breast exams and mammograms to screen for breast cancer. Mammograms can be more difficult to interpret in women with dense breasts, so it is important to find a radiologist who is experienced in interpreting mammograms in women with diabetic mastopathy.
Tip 5: Talk to your doctor about medications. There are a number of medications that can help to manage diabetic mastopathy. These medications can help to reduce breast pain and swelling, and they can also help to prevent the development of breast cancer.
Summary: Diabetic mastopathy is a common condition that can affect women with diabetes. By following these tips, women can help to manage the condition and reduce their risk of breast cancer.
Transition to the article’s conclusion: For more information on diabetic mastopathy, please consult with your healthcare provider or visit a reputable medical website.
Diabetic Mastopathy
Diabetic mastopathy is a condition that can affect women with diabetes. It is characterized by the presence of dense, fibrous tissue in the breasts, which can make it more difficult to detect breast cancer on mammograms. While there is no cure for diabetic mastopathy, there are a number of things that women can do to manage the condition and reduce their risk of breast cancer.
It is important for women with diabetes to be aware of the symptoms of diabetic mastopathy and to have regular breast exams and mammograms. Early detection and treatment of breast cancer is essential for improving the chances of a successful outcome.
Youtube Video: