Diabetes measurement refers to the process of monitoring and assessing blood glucose (sugar) levels in individuals with diabetes. It involves using specialized devices, such as blood glucose meters, to measure the amount of glucose present in a sample of blood, usually taken from a fingertip.
Regular diabetes measurement is crucial for effective diabetes management. It allows individuals to track their blood glucose levels over time, identify patterns, and make informed decisions about their diet, medication, and lifestyle choices. By maintaining optimal glucose control, individuals can reduce the risk of developing diabetes-related complications, such as heart disease, stroke, kidney failure, and blindness.
Historically, diabetes measurement has evolved significantly. In the past, individuals with diabetes relied on urine tests to assess their glucose levels, which were less accurate and required more frequent testing. With advancements in technology, blood glucose meters have become more accessible, affordable, and user-friendly, enabling individuals to perform self-monitoring of their blood glucose levels conveniently and accurately.
Diabetes Measurement
Diabetes measurement is a crucial aspect of diabetes management, involving the monitoring and assessment of blood glucose levels. Key aspects of diabetes measurement include:
- Accuracy
- Frequency
- Timing
- Method
- Interpretation
- Communication
Accuracy in diabetes measurement is essential to ensure reliable results. Regular and frequent measurements help identify patterns and trends in blood glucose levels. Appropriate timing of measurements, such as before and after meals, exercise, or bedtime, provides a comprehensive picture of glucose control. The method of measurement, whether using blood glucose meters, continuous glucose monitors, or laboratory tests, should align with individual needs and preferences. Correct interpretation of measurement results is crucial for making informed decisions about diabetes management. Effective communication between individuals with diabetes and healthcare professionals is vital to convey measurement results and adjust treatment plans accordingly.
Accuracy
Accuracy in diabetes measurement is of paramount importance as it directly impacts the quality of diabetes management and the well-being of individuals. Inaccurate measurements can lead to misinterpretation of blood glucose levels, resulting in inappropriate treatment decisions and potentially severe consequences.
Accurate diabetes measurement enables individuals to make informed choices about their insulin dosage, diet, and lifestyle. It helps them identify patterns and trends in their blood glucose levels, anticipate and prevent hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar), and adjust their treatment plans accordingly. Accurate measurements also facilitate timely interventions by healthcare professionals, ensuring optimal diabetes management and reducing the risk of long-term complications.
To ensure accuracy in diabetes measurement, individuals should use well-calibrated and reliable blood glucose meters. Proper technique, such as washing hands before testing and using the correct test strips, is essential. Regular calibration of meters using control solutions is also crucial to maintain accuracy. Additionally, individuals should be trained on the correct use of their meters and consult with their healthcare team for guidance and support.
Frequency
Frequency of diabetes measurement is a critical aspect of effective diabetes management. Regular and frequent measurements provide individuals with a comprehensive understanding of their blood glucose patterns and trends, enabling them to make informed decisions about their treatment and lifestyle.
The frequency of diabetes measurement varies depending on individual factors such as the type of diabetes, treatment regimen, and overall health status. However, it is generally recommended that individuals with diabetes measure their blood glucose levels multiple times per day, including before and after meals, before and after exercise, and at bedtime. This frequent monitoring helps identify patterns and trends, anticipate and prevent hypoglycemia or hyperglycemia, and adjust treatment plans accordingly.
Consistent and frequent diabetes measurement enables individuals to identify patterns and trends in their blood glucose levels, which can vary significantly throughout the day. This information is crucial for optimizing insulin dosage, diet, and lifestyle choices. It also facilitates timely interventions by healthcare professionals, ensuring optimal diabetes management and reducing the risk of long-term complications.
Timing
Timing plays a crucial role in diabetes measurement, influencing the accuracy and effectiveness of blood glucose monitoring. Key aspects to consider include:
- Pre-Meal and Post-Meal Measurements: Measuring blood glucose levels before and after meals provides valuable insights into the impact of food on blood sugar levels. It helps individuals identify foods that cause blood sugar spikes and adjust their diet accordingly.
- Fasting Measurements: Fasting blood glucose measurements, typically taken in the morning before eating or drinking anything, reflect the body’s baseline glucose levels. They are useful for assessing the effectiveness of diabetes medication and overall diabetes management.
- Bedtime Measurements: Measuring blood glucose levels at bedtime helps individuals identify potential overnight hypoglycemia or hyperglycemia. This information guides adjustments to insulin dosage or bedtime snacks to prevent blood sugar fluctuations during sleep.
- Exercise Measurements: Exercise can significantly impact blood glucose levels. Measuring blood glucose before, during, and after exercise helps individuals understand how their body responds to physical activity and adjust their insulin or medication accordingly.
Appropriate timing of diabetes measurement empowers individuals to make informed decisions about their diabetes management. By considering the timing of measurements in relation to meals, sleep, and exercise, they can optimize their treatment plans, prevent complications, and improve their overall health outcomes.
Method
The method of diabetes measurement significantly impacts the accuracy, reliability, and convenience of blood glucose monitoring. Individuals have various options to choose from, each with its own advantages and considerations.
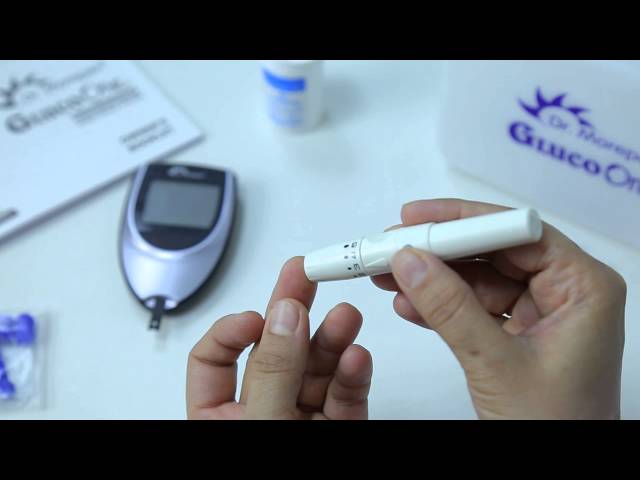
Blood Glucose Meters: Blood glucose meters are portable devices that measure glucose levels in a small sample of blood, usually obtained from a fingertip. They are commonly used for self-monitoring of blood glucose levels and provide quick and convenient results.
Continuous Glucose Monitors (CGMs): CGMs are small, wearable devices that continuously measure glucose levels in interstitial fluid, which is just beneath the skin. They provide real-time glucose readings and can alert individuals to potential highs or lows, offering more comprehensive glucose monitoring.
Laboratory Tests: Laboratory tests, such as the A1C test, measure average blood glucose levels over a period of time, typically the past 2-3 months. A1C tests are useful for assessing long-term glucose control and are often used by healthcare professionals to monitor diabetes management.
The choice of diabetes measurement method depends on individual needs, lifestyle, and preferences. It is essential to consult with a healthcare professional to determine the most appropriate method and ensure accurate and effective diabetes management.
Interpretation
Interpretation of diabetes measurement results is a critical aspect of effective diabetes management. Individuals need to understand the meaning of their blood glucose readings to make informed decisions about their treatment and lifestyle. Proper interpretation involves recognizing patterns, identifying trends, and understanding the implications of glucose levels.
- Understanding Patterns: Tracking blood glucose measurements over time helps individuals identify patterns in their glucose levels. They can observe how different foods, activities, and medications affect their blood sugar and adjust their management accordingly.
- Identifying Trends: Beyond daily fluctuations, analyzing blood glucose measurements over longer periods can reveal trends. Individuals may notice gradual increases or decreases in their glucose levels, which could indicate changes in their overall diabetes management or underlying health conditions.
- Recognizing Implications: Interpreting blood glucose measurements involves understanding their implications for diabetes management. High blood sugar levels may indicate the need for medication adjustments or lifestyle changes, while low blood sugar levels require immediate attention to prevent hypoglycemia.
- Communicating with Healthcare Providers: Accurate interpretation of diabetes measurement results is crucial for effective communication with healthcare providers. Individuals should be able to clearly convey their blood glucose patterns and trends to their healthcare team, who can then provide guidance and support.
Proper interpretation of diabetes measurement results empowers individuals to take an active role in managing their condition. By understanding the meaning of their blood glucose readings, they can make informed decisions about their treatment, lifestyle, and overall health.
Communication
Communication plays a vital role in diabetes measurement, as it enables individuals to effectively convey their blood glucose readings and patterns to healthcare providers. Clear and accurate communication is essential for healthcare providers to assess an individual’s diabetes management, identify potential issues, and provide appropriate guidance and support.
Individuals with diabetes should be able to communicate their blood glucose measurements, including patterns and trends, to their healthcare team. This information helps healthcare providers make informed decisions about treatment plans, medication adjustments, and lifestyle recommendations tailored to each individual’s needs.
Effective communication also involves individuals asking questions, expressing concerns, and actively participating in their diabetes management plan. Open and honest communication between individuals with diabetes and their healthcare providers is crucial for achieving optimal diabetes outcomes.
FAQs on Diabetes Measurement
This section addresses frequently asked questions (FAQs) related to diabetes measurement, providing informative answers to common concerns and misconceptions.
Question 1: Why is diabetes measurement important?
Answer: Diabetes measurement is essential for effective diabetes management. It allows individuals to monitor their blood glucose levels, identify patterns, and make informed decisions about their diet, medication, and lifestyle choices. Regular diabetes measurement helps prevent complications and optimizes overall health outcomes.
Question 2: How often should I measure my blood glucose levels?
Answer: The frequency of diabetes measurement varies depending on individual factors, but generally, it is recommended to measure blood glucose levels multiple times per day, including before and after meals, before and after exercise, and at bedtime. Consistent and frequent monitoring provides a comprehensive understanding of glucose patterns and trends.
Question 3: What is the best method for diabetes measurement?
Answer: The choice of diabetes measurement method depends on individual needs and preferences. Common methods include blood glucose meters, continuous glucose monitors (CGMs), and laboratory tests. Blood glucose meters are portable and convenient for self-monitoring, CGMs provide real-time glucose readings, and laboratory tests offer long-term glucose control assessment.
Question 4: How can I interpret my diabetes measurement results?
Answer: Interpreting diabetes measurement results involves understanding patterns, identifying trends, and recognizing implications. Individuals should track their blood glucose readings over time to identify how different factors affect their glucose levels. High blood sugar levels may indicate the need for medication adjustments, while low blood sugar levels require immediate attention.
Question 5: Why is communication important in diabetes measurement?
Answer: Effective communication between individuals with diabetes and their healthcare providers is crucial for diabetes measurement. Clear and accurate communication ensures that healthcare providers have a comprehensive understanding of an individual’s blood glucose patterns and can provide appropriate guidance, support, and treatment plans.
Question 6: What are some tips for effective diabetes measurement?
Answer: To ensure accurate and effective diabetes measurement, individuals should use well-calibrated blood glucose meters, follow proper testing techniques, and maintain a consistent measurement schedule. Additionally, understanding the implications of blood glucose readings and communicating them effectively to healthcare providers is essential for optimal diabetes management.
Summary: Diabetes measurement is a crucial aspect of diabetes management, empowering individuals to monitor their blood glucose levels, identify patterns, and make informed decisions about their health. By understanding the importance of diabetes measurement, choosing the appropriate method, interpreting results effectively, and communicating clearly with healthcare providers, individuals can optimize their diabetes management and achieve better health outcomes.
Transition to the next article section: This concludes the FAQs on diabetes measurement. The following section will delve into advanced topics related to diabetes management.
Diabetes Measurement Tips
To ensure accurate and effective diabetes measurement, individuals should follow these essential tips:
Tip 1: Calibrate Your Blood Glucose Meter: Regularly calibrate your blood glucose meter using a control solution to ensure accuracy. This process adjusts the meter to provide reliable blood glucose readings.
Tip 2: Use Proper Technique: When testing your blood glucose, follow the manufacturer’s instructions carefully. Wash your hands, use the correct test strip, and obtain the blood sample from the designated area.
Tip 3: Test Consistently: Consistency in blood glucose measurement is vital. Follow your recommended testing schedule and record your results to track patterns and trends.
Tip 4: Consider a Continuous Glucose Monitor (CGM): A CGM provides real-time glucose readings and can alert you to potential highs or lows. Discuss with your healthcare provider if a CGM would benefit your diabetes management.
Tip 5: Understand Your Blood Glucose Levels: Learn what your target blood glucose range is and recognize the signs and symptoms of high or low blood sugar. This knowledge empowers you to make informed decisions about your diabetes management.
Tip 6: Communicate Effectively: Clearly communicate your blood glucose readings and patterns to your healthcare provider. This information helps them assess your diabetes management and make necessary adjustments to your treatment plan.
Summary: By following these tips, individuals with diabetes can ensure accurate and effective diabetes measurement, enabling them to optimize their diabetes management and achieve better health outcomes.
Transition to the article’s conclusion: These diabetes measurement tips empower individuals to take an active role in their health and work closely with their healthcare providers to manage their condition effectively.
Conclusion
Diabetes measurement is a fundamental aspect of effective diabetes management, providing individuals with the means to monitor their blood glucose levels and make informed decisions about their health. This article has explored the various aspects of diabetes measurement, including its importance, methods, interpretation, and communication.
By understanding the significance of diabetes measurement, individuals can actively participate in their diabetes management, identify patterns and trends, and work closely with their healthcare providers to optimize their treatment plans. Accurate and consistent diabetes measurement empowers individuals to prevent complications, improve their overall health outcomes, and live fulfilling lives with diabetes.
Youtube Video: