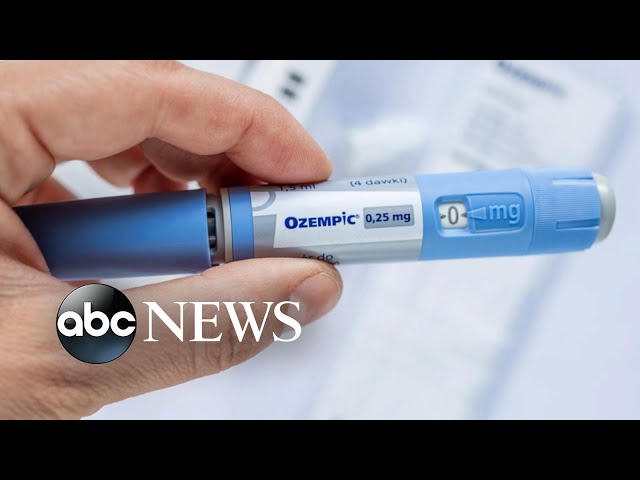
Diabetes injection medicine is a medication used to treat diabetes. It is injected into the body, usually subcutaneously (under the skin). Diabetes injection medicine works by helping the body to produce more insulin or by making the body more sensitive to insulin, which is a hormone that helps the body to use glucose (sugar) for energy.
Diabetes injection medicine is an important treatment option for people with diabetes. It can help to control blood sugar levels and prevent serious complications, such as heart disease, stroke, kidney disease, and blindness. Diabetes injection medicine is also relatively safe and well-tolerated.
There are many different types of diabetes injection medicine available. The type of medicine that is best for a particular person will depend on their individual needs and preferences. Some of the most common types of diabetes injection medicine include:
- Insulin
- Glucagon-like peptide-1 (GLP-1) agonists
- Dipeptidyl peptidase-4 (DPP-4) inhibitors
- Sodium-glucose cotransporter 2 (SGLT2) inhibitors
diabetes injection medicine
Diabetes injection medicine is a crucial treatment option for managing blood sugar levels and preventing serious health complications in individuals with diabetes. Key aspects related to diabetes injection medicine include:
- Types: Various types of injection medicines are available, including insulin, GLP-1 agonists, DPP-4 inhibitors, and SGLT2 inhibitors.
- Mechanism: These medicines work by increasing insulin production, enhancing insulin sensitivity, or reducing glucose reabsorption in the kidneys.
- Administration: Injected subcutaneously, these medicines provide precise and controlled delivery of medication.
- Benefits: Injection medicines effectively lower blood sugar levels, reduce the risk of complications, and improve overall well-being.
- Monitoring: Regular blood sugar monitoring and medical check-ups are essential to optimize treatment and prevent adverse effects.
- Lifestyle: Diabetes injection medicine complements a healthy lifestyle that includes proper diet, exercise, and stress management.
In conclusion, diabetes injection medicine offers a range of options to tailor treatment to individual needs. By understanding the types, mechanisms, administration, benefits, monitoring, and lifestyle considerations associated with these medicines, individuals with diabetes can effectively manage their condition and improve their quality of life.
Types
The availability of various types of injection medicines is a crucial aspect of diabetes injection medicine. These different types target specific mechanisms involved in diabetes, allowing for tailored treatment approaches based on individual patient needs and characteristics.
For instance, insulin is essential for individuals with Type 1 diabetes, where the body produces little to no insulin. GLP-1 agonists stimulate insulin production and slow down gastric emptying, making them beneficial for managing post-meal glucose levels. DPP-4 inhibitors enhance the effects of incretin hormones, which stimulate insulin secretion and reduce glucagon release. SGLT2 inhibitors work by reducing glucose reabsorption in the kidneys, leading to increased glucose excretion in the urine.
The availability of these diverse injection medicines empowers healthcare providers to personalize treatment plans, optimize blood sugar control, and minimize the risk of long-term complications associated with diabetes. Understanding the specific mechanisms and indications for each type of injection medicine is paramount for effective diabetes management.
Mechanism
Understanding the mechanism of action is fundamental to comprehending the role of diabetes injection medicine in managing blood sugar levels. These medicines exert their effects through various pathways, including increasing insulin production, enhancing insulin sensitivity, or reducing glucose reabsorption in the kidneys.
Insulin is a hormone produced by the pancreas that enables the body to utilize glucose for energy. In individuals with diabetes, the body either produces insufficient insulin (Type 1 diabetes) or does not respond adequately to insulin (Type 2 diabetes). Diabetes injection medicine addresses these issues by increasing insulin production or enhancing insulin sensitivity, allowing glucose to be taken up and utilized by cells more effectively.
Another mechanism involves reducing glucose reabsorption in the kidneys. The kidneys play a crucial role in regulating blood sugar levels by reabsorbing glucose from the urine back into the bloodstream. SGLT2 inhibitors, a class of diabetes injection medicine, block the SGLT2 protein in the kidneys, leading to increased glucose excretion in the urine and, consequently, lower blood sugar levels.
By targeting specific mechanisms, diabetes injection medicine provides a targeted approach to managing diabetes. This understanding empowers healthcare providers to tailor treatment plans based on individual patient needs and characteristics, ultimately optimizing blood sugar control and reducing the risk of long-term complications associated with diabetes.
Administration
Subcutaneous injection is a crucial aspect of diabetes injection medicine, as it enables precise and controlled delivery of medication directly into the body’s fatty tissue beneath the skin. This method of administration offers several advantages that are essential for effective diabetes management.
Firstly, subcutaneous injection bypasses the digestive system, ensuring that the medication is not broken down or absorbed in the stomach and intestines. This allows for more accurate and reliable absorption of the medication into the bloodstream, resulting in consistent and predictable blood sugar control.
Secondly, subcutaneous injection provides a sustained release of medication over time, which helps to maintain stable blood sugar levels throughout the day. This is particularly important for individuals with diabetes who require continuous insulin therapy or other long-acting medications.
Moreover, subcutaneous injection allows for flexible administration, as it can be performed at any time and in any location. This flexibility empowers individuals with diabetes to manage their condition discreetly and conveniently, without disrupting their daily routine.
In summary, the subcutaneous administration of diabetes injection medicine is a critical component of effective diabetes management. It ensures precise and controlled delivery of medication, sustained release over time, and flexible administration, ultimately contributing to optimal blood sugar control and improved quality of life for individuals with diabetes.
Benefits
The benefits of diabetes injection medicine are closely tied to its ability to effectively lower blood sugar levels, reduce the risk of complications, and improve overall well-being. This connection is crucial for understanding the significance of injection medicines in diabetes management.
Firstly, injection medicines play a critical role in controlling blood sugar levels. By increasing insulin production or enhancing insulin sensitivity, these medicines enable the body to utilize glucose more efficiently, leading to lower blood sugar levels. This is essential for preventing acute complications such as diabetic ketoacidosis or hypoglycemia, as well as long-term complications such as cardiovascular disease, stroke, and kidney failure.
Secondly, injection medicines significantly reduce the risk of developing diabetes-related complications. By maintaining stable blood sugar levels, these medicines help protect various organs and tissues from damage. For instance, they reduce the risk of retinopathy, a leading cause of blindness in individuals with diabetes, as well as neuropathy, a condition that affects the nerves.
Moreover, injection medicines contribute to improving overall well-being in individuals with diabetes. By effectively managing blood sugar levels and reducing the risk of complications, these medicines enhance quality of life. Individuals experience fewer symptoms such as fatigue, thirst, and frequent urination, and they have increased energy levels and a better sense of general health.
In conclusion, the benefits of diabetes injection medicine are far-reaching, impacting both physical and overall well-being. These medicines effectively lower blood sugar levels, reduce the risk of complications, and improve quality of life, making them a cornerstone of diabetes management.
Monitoring
Monitoring blood sugar levels and attending regular medical check-ups are crucial components of diabetes injection medicine. This connection stems from the need to optimize treatment and prevent adverse effects, ensuring the safe and effective use of these medications.
Regular blood sugar monitoring allows individuals to track the impact of their injection medicine and make necessary adjustments to their dosage or lifestyle. By identifying patterns and trends in their blood sugar levels, they can work with their healthcare provider to personalize their treatment plan and achieve optimal glycemic control. This monitoring also helps detect potential adverse effects, such as hypoglycemia, and enables prompt intervention to prevent serious complications.
Medical check-ups are equally important, as they provide a comprehensive assessment of an individual’s overall health and diabetes management. These check-ups involve physical examinations, blood tests, and discussions about medication adherence, lifestyle factors, and any concerns or challenges faced. Through these check-ups, healthcare providers can evaluate the effectiveness of injection medicine, monitor for potential side effects, and make necessary adjustments to the treatment plan. They also provide an opportunity for individuals to receive education, support, and guidance on managing their diabetes effectively.
In summary, monitoring blood sugar levels and attending regular medical check-ups are essential aspects of diabetes injection medicine. They empower individuals to actively participate in their diabetes management, optimize treatment outcomes, and prevent adverse effects. This understanding is crucial for ensuring the safe and effective use of injection medicines and improving the overall well-being of individuals with diabetes.
Lifestyle
Diabetes injection medicine forms a crucial part of a comprehensive diabetes management plan that encompasses not just medication, but also lifestyle modifications. Proper diet, regular exercise, and effective stress management play a vital role in optimizing the effects of diabetes injection medicine and improving overall health outcomes.
-
Dietary Considerations:
Maintaining a balanced and nutritious diet is essential for individuals with diabetes. A healthy diet helps control blood sugar levels, reduce the risk of heart disease and other complications, and support overall well-being. Diabetes injection medicine can enhance the effects of dietary changes, making it easier to manage blood sugar levels and achieve glycemic goals.
-
Regular Exercise:
Engaging in regular physical activity is crucial for individuals with diabetes. Exercise improves insulin sensitivity, helps control blood sugar levels, and promotes overall cardiovascular health. Diabetes injection medicine can complement an exercise program by enhancing the body’s ability to utilize glucose during physical activity, leading to improved glycemic control and increased energy levels.
-
Stress Management:
Stress can significantly impact blood sugar levels in individuals with diabetes. Effective stress management techniques, such as yoga, meditation, or deep breathing exercises, can help reduce stress levels and improve overall well-being. Diabetes injection medicine can provide additional support in managing stress-induced blood sugar fluctuations, contributing to better overall diabetes management.
In summary, diabetes injection medicine works synergistically with a healthy lifestyle that includes proper diet, exercise, and stress management. By adopting these lifestyle modifications, individuals with diabetes can maximize the benefits of their medication, improve their overall health, and reduce the risk of long-term complications.
FAQs on Diabetes Injection Medicine
Diabetes injection medicine is a vital part of diabetes management, and it’s natural to have questions about its use. Here are answers to some frequently asked questions:
Question 1: How does diabetes injection medicine work?
Diabetes injection medicine works by regulating blood sugar levels. It either increases insulin production, enhances insulin sensitivity, or reduces glucose reabsorption in the kidneys, depending on the specific type of medicine.
Question 2: Is diabetes injection medicine safe?
Yes, diabetes injection medicine is generally safe when used as directed by a healthcare professional. However, it’s important to monitor blood sugar levels regularly and report any adverse effects to your doctor.
Question 3: How often do I need to inject diabetes medicine?
The frequency of injections varies depending on the type of medicine and individual needs. Your doctor will determine the appropriate dosing schedule for you.
Question 4: Can I take diabetes injection medicine with other medications?
Always consult your doctor before combining diabetes injection medicine with other medications, as some interactions may occur.
Question 5: What are the potential side effects of diabetes injection medicine?
Common side effects include injection site reactions, low blood sugar (hypoglycemia), and weight gain. More serious side effects are rare but can occur.
Question 6: How can I manage my diabetes effectively with injection medicine?
Effective diabetes management involves using injection medicine as prescribed, monitoring blood sugar levels, following a healthy diet, exercising regularly, managing stress, and attending regular medical check-ups.
These FAQs provide a general overview, and it’s essential to consult your healthcare provider for personalized guidance on diabetes injection medicine and overall diabetes management.
Transition to the next article section: Understanding the Types of Diabetes Injection Medicine
Tips for Using Diabetes Injection Medicine
To ensure safe and effective use of diabetes injection medicine, follow these essential tips:
Tip 1: Proper Injection Technique
Use the correct injection technique to prevent infection and ensure accurate medication delivery. Clean the injection site, inject at a 90-degree angle, and rotate injection sites regularly.
Tip 2: Monitor Blood Sugar Levels
Regular blood sugar monitoring is crucial to assess the effectiveness of your medication and adjust dosage as needed. Consult your healthcare provider to determine an appropriate monitoring schedule.
Tip 3: Manage Diet and Exercise
Maintain a healthy diet and engage in regular physical activity to complement the effects of diabetes injection medicine. This helps control blood sugar levels and improves overall well-being.
Tip 4: Store Medicine Properly
Store diabetes injection medicine according to the manufacturer’s instructions. Protect it from extreme temperatures and light to maintain its potency and efficacy.
Tip 5: Avoid Alcohol and Smoking
Excessive alcohol consumption and smoking can interfere with blood sugar control and negate the benefits of diabetes injection medicine. It’s best to avoid or limit these substances.
Tip 6: Report Side Effects
Monitor for potential side effects and report any concerns to your healthcare provider promptly. They can assess the severity and make necessary adjustments to your treatment plan.
Tip 7: Follow-Up Appointments
Attend regular follow-up appointments with your healthcare provider to review your progress, adjust medications if needed, and receive ongoing support and guidance.
Following these tips can optimize the effectiveness and safety of diabetes injection medicine, leading to better blood sugar control and improved overall health.
Transition to the article’s conclusion: The Importance of Adhering to Diabetes Injection Medicine
Conclusion
Diabetes injection medicine plays a crucial role in managing blood sugar levels and improving the quality of life for individuals with diabetes. This article has explored the various aspects of diabetes injection medicine, including its types, mechanisms of action, administration, benefits, monitoring, lifestyle considerations, and essential tips for usage.
Effective diabetes management requires a comprehensive approach that combines medication, lifestyle modifications, and regular monitoring. Diabetes injection medicine is a powerful tool that, when used correctly and in conjunction with other strategies, can significantly improve blood sugar control, reduce the risk of complications, and promote overall well-being. By adhering to prescribed treatment plans, monitoring blood sugar levels, and making healthy lifestyle choices, individuals with diabetes can harness the full benefits of diabetes injection medicine and live healthier, more fulfilling lives.
Youtube Video: